Pet Health Tips: General
- Annual Physical Exam
- Bloodwork
- Cold Injuries
- Heartworm Preventative
- Cranial Cruciate Ligament Rupture
- Dental Prophylaxis
- Dry Eye
- Epistaxis
- Flatulence
- Flea Control
- Glaucoma
- Have a Safe Trip
- Heartworm Disease
- Hyperparathyroidism
- Hyperthemia
- Pilling Your Pet
- Senior Wellness
- Traveling
- Trimming Your Pet's Nails
- Understanding Your Pet's Bloodwork
- Valley Fever
- What is this Lump?
The Annual Physical Exam, Not the Annual Vaccinations
Too often in veterinary medicine the emphasis placed on vaccinating your animals every year is over-emphasized. However, without vaccines, a deadly zoonotic disease like rabies would still be prevalent in the human and companion animal population. With new developments in vaccine creation, delivery, and understanding of longevity, vaccination is no longer a necessity every year in all cases. It is still important for your animal to see their veterinarian every year. An annual physical exam for your animal is as important as an annual physical exam for yourself. It is at these times that preventative medicine, and not reactionary medicine, can be implemented to its fullest. The suspicion and possible follow up diagnosis of orthopedic, endocrine, gastrointestinal, and dermatologic diseases allows conservative therapy to be instituted before things like costly surgery, or expensive medications are necessary. The annual physical exam is your veterinarians #1 tool in providing the best long term care for your pets. So remember, your annual visit to your veterinarian’s office is not just for vaccinations, it’s for the long term health of the most important four legged members of your family.
Blood Work: Special Considerations for the Older Pet
By Tammy Marheine
Our older cats and dogs have special needs just as we do when we age. It is often recommended that in addition to the routine wellness exam and vaccinations that cats and dogs receive every year, that special blood work be considered. As our pets age, they become more prone to conditions affecting their internal organs such as their kidneys and liver. Blood work is always recommended prior to anesthesia or when a problem is suspected. Once our pets reach the age of six or seven years (depending on breed and previous medical history) a yearly blood chemistry, CBC, and urinalysis are strongly advised to evaluate internal organ function. These tests should be performed in addition to the recommended yearly heartworm test and fecal exam. We also suggest that older dogs that have exhibited weight gain or a change in their activity level receive thyroid hormone screening to rule out hypothyroidism, or a deficiency in thyroid hormone. Older cats are prone to hyperthyroidism, a condition in which too much thyroid hormone is produced. As a result, it is suggested that thyroid hormone levels also be measured in our senior cats. The specific screening tests that will be performed on your pet will be decided by you and your veterinarian, and will often vary from animal to animal. It is important that you and your veterinarian discuss the care of your older pet and design a wellness program to fit his or her specific needs. Our senior pets are very special and have often been in the family for many years.
Cold injuries (Frostbite)
Frostbite is the death of local tissue due to exposition of extremities to severe and prolonged cold. The most affected areas are: ear, tail, scrotum, mammary gland, digits, and flanks because these regions are covered with sparse hair, and have poor peripheral circulation.
The diagnosis of frostbite is determined with history of exposure to severe or prolonged cold, and inspection of the affected area, where the frozen tissue is pale and cool in contrast with healthy tissue The healthy tissue is red, painful, and scaly. The dead tissue may present severe complications, such as gangrene or mummification and sloughs if is not treated correctly.
Frostbite can be further classified in:
- 1) Superficial: only skin is affected.
- 2) Deep: skin, and deep tissue belong it.
Treatment:
- Immediate treatment includes slow rewarming by moist heat applications at 102F to 107F for twenty minutes or by immersion in warm water.
- Affected areas can be treated with aloe vera or silver sulfadiazine.
- The areas can be painful and analgesics may be needed to alleviate pain and administration of prophylactic antibiotic must be considered.
- Conservative therapy should be used for three to six weeks, until healthy tissue can be distinguished from dead tissue.
- Do not use corticosteroids and do not amputate, because many tissues recover.
- Bandage can be used to prevent self trauma.
- Necrotic tissue should then be debrided and the area reconstructed if necessary.
- Intravascular coagulation is a common problem; this problem must be addressed by a veterinarian.
Frequently Asked Questions about Heartworm Preventative
By Jessica Maloney
How does Heartworm Preventative Work?
Heartworm preventatives do not actually prevent mosquitoes from infecting your dog with heartworm larvae. These preventatives actually kill different stages of heartworm larvae that already have infected your dog. Different types of heartworm preventatives kill different stages of heartworm larvae. Therefore heartworm preventatives can have different schedules of administration (monthly or every 6 months).
Why does my dog need to be tested for heartworms every year even though he’s been on heartworm prevention?
There are several reasons that dogs need to be tested every year for heartworm. Monthly administration of heartworm preventative is generally easy, however seldomly dogs can vomit up the chewable tablets or spit them out with out you noticing, leaving the dog unprotected. Dogs also need to be tested every year, because depending on which preventative your dog is on, it can be dangerous to give your dog preventative if he is infected with adult heartworms. Another great reason to test your dog is if there has been product failure (i.e. you have given heartworm preventative religiously and your dog is diagnosed with heartworm disease), most companies that produce heartworm preventatives have a guarantee on their product and will pay for any treatment necessary for your dog.
Why should my dog be on heartworm prevention year round?
Your dog should be on heartworm preventative all year for many reasons. Due to seasonal variation, areas like Indiana generally do not have a mosquito population during the cold winter months. However, we all know that Indiana weather is not predictable and warm weather can occur at any time. This unpredictability can lead to lingering mosquito populations and risk of infection to your dog if he is not on heartworm preventative year round. Heartworm preventatives can also treat and prevent some intestinal parasitic diseases like hookworm, roundworm, and whipworm infestations. Not all preventatives treat these other parasites, so be sure to ask your veterinarian which preventatives are right for your dog. And finally, it is good to keep your dog on year-round prevention simply in order to stay in the habit of administering the medication to your dog monthly or every 6 months.
What heartworm preventatives are available?
| How often does my dog receive the preventative? | How is the preventative given? | What parasites is the preventative effective against in dogs? | |
|---|---|---|---|
| Heartguard (ivermectin) | Monthly | By mouth | Heartworms |
| Heartguard Plus (ivermectin + pyrantel) | Monthly | By mouth | Heartworms, hookworms, roundworms |
| Interceptor (milbemycin oxime) | Monthly | By mouth | Heartworms, hookworms, roundworms, whipworms |
| Sentinel (milbemycin oxime + lufenuron) | Monthly | By mouth | Heartworms, hookworms, roundworms, whipworms, flea reproduction |
| Advantage Multi (moxidectin /imidicloprid) | Monthly | Topical | Fleas, heartworms, hookworms |
| Revolution (selamectin) | Monthly | Topical | Heartworms, fleas, ticks, ear mites, sarcoptes |
Cranial cruciate ligament rupture
by Rajeev Nair
Cranial cruciate ligament (CCL) rupture is the tearing of an important ligament in the stifle joint (knee), resulting in partial or complete joint instability, pain, and lameness. Torn ligaments retract, do not heal, and cannot be repaired. CCL rupture occurs in both dogs and cats. CCL rupture occurs more frequently in dogs than in cats. CCL is one of the most common orthopedic injuries in dogs and is the most common cause of degenerative joint disease in the stifle joint. CCL rupture occurs in dogs of all sizes, but is most prevalent in large and giant breeds.
The knee joint of the dog is one of the weakest in the body. Just as football players frequently suffer knee injuries, the dog may also be prone to knee injuries. The two main bones, the femur and tibia, are joined with several ligaments. Four major ligaments (dense bands of fiber) support and stabilize the stifle joint by connecting the femur to the tibia and the joint capsule to the bones. The medial and lateral collateral ligaments are located outside the joint and the caudal and cranial cruciate ligaments are located inside the joint. The CCL attaches to the femur, runs across the stifle joint, and attaches to the tibia. The CCL holds the tibia in place and prevents internal rotation and hyperextension.
Rupture of the CCL is caused by sudden, severe twisting of the ligament. The injury usually occurs when the animal steps in a hole while running or turns with its paw remaining planted. The twisting motion causes the ligament to hyperextend or rotates excessively and leads to a complete or partial rupture. The meniscus (cartilage) is often damaged as well. Chronic rupture occurs after the ligament has degenerated with age. The fibers weaken and partially tear, the joint becomes unstable, and degenerative joint disease develops. A partially torn CCL eventually tears completely.
The usual signs noticed in dogs and cats are lameness of affected leg, instability of the joint and abnormal movement of the bones in relation to each other causing pain and discomfort. It is not possible to bear weight on the leg without discomfort or pain. The most reliable means of diagnosing this injury is to move the femur and tibia in a certain way to demonstrate the instability. This movement is called a "drawer sign." It can usually be demonstrated with the dog awake. If the dog is experiencing severe pain, has very strong leg muscles, or is uncooperative, it may be necessary to use sedation in order to examine the joint thoroughly. Correction of this problem requires surgery. A skilled surgeon can fashion a replacement ligament and stabilize the joint so it functions normally or near normally. If surgery is not performed within a few days to a week, arthritic changes will begin that cannot be reversed, even with surgery. Over weight dogs may require special diets for weight control.
Dental Prophylaxis
Like humans, dogs’ teeth need to be cleaned regularly. Bacteria in the mouth combined with saliva and food debris between the gum and teeth can cause plaque accumulation on the tooth. As mineral salts are deposited, plaque turns to tartar. Without proper care and treatment, this plaque and tartar build up can damage the gums and teeth leading to gum disease and periodontal disease which affects the tissue and structure supporting the teeth. The disease causes red, swollen and tender gums, bleeding, pain and bad breath. If left untreated, periodontitis can lead to tooth loss. The infection caused by periodontal disease may enter the blood stream potentially infecting the heart, liver and kidneys. How could you prevent your pet's dental diseases? The first step in preventing oral disease is a routine dental exam by your veterinarian. Dog owners should practice a routine dental care procedure at home to prevent dental diseases. Home care encompasses brushing, special dental diets, chew toys, hygienic solutions and gels. Brushing should be done using a pet toothbrush with the specially formulated tooth paste such as flavored enzymatic tooth paste (C.E.T) or Maxigard gel.
The first step in brushing is getting the pet accustomed to being gently handled around the face by rubbing the sides of the cheek, petting under the chin etc.
Next the owner should start carefully lifting the lips and lightly touching the gums and teeth with a gauze sponge or soft cloth. Later, a pet tooth brush can be used.
Dry Eye
What is dry eye?
Keratoconjunctivitis sicca (KCS). KCS is a disease in which there is a decrease in the amount of tears secreted by the eye. It typically is first seen in only one eye, but often will eventually involve both eyes.
What is the function of tears?
Tears bathe the eye keeping it moist, which provides the eye with nutrients and oxygen, and helps to protect the eye from the environment.
What clinical signs would you see in a dog with dry eye?
The eye would be painful (pawing at the eye, blinking), redness, excessive amount of clear or yellow mucous-like discharge, and sometimes a dry, crusty nose.
How do you diagnose KCS?
The first clinical signs the animal usually presents with would be blinking, and pawing at the affected eye which often indicates KCS. Next, a Schirmer tear test would be performed. This is a piece of paper labeled in millimeters that is placed in the eye for one minute. Tears move down the strip, turning the paper blue, indicating the amount of tears made. Below 10mm of tear production is strongly indicative of KCS. Above 15mm is considered normal.
What is the treatment for KCS?
Most cases of KCS require a life-long commitment by the owners. This disease can be managed, but never cured. Treatments include:
- Optimmune (Cyclosporine): Stimulates tear production and decreases inflammation. It comes as an ointment, drops, or an oral suspension, and is usually given twice a day.
- Artificial tears: Helps keep the eye moist and lubricated. It comes as a drop or an ointment. The drops are usually given every 1-2 hours and ointment every 3-4 hours.
What if the medical treatments fail to help my pet?
If after 2 months of medical treatment, there is no improvement with the KCS, there is a surgical option. There is a procedure called Parotid Duct Transposition, in which a salivary gland is used to help lubricate the eye.
What secondary complications can arise from KCS?
One possible secondary complication is an ulcer on the eye. Flourescein stain test is used to check the eye for ulcers. The dye strip is moistened with eye wash solution. Then the strip is placed on the eye briefly to deposit the stain, which is a bright yellow-green color. Next, the eye is rinsed with eye wash solution. The eye will then be examined with an ophthalmoscope. Any stain still present on the eye indicates an area of ulceration. Be aware that it is normal to see some yellow-green fluid dripping from your pet’s nose after this test is performed.
Other possible complications include bacterial infection of the eye, and patches of color on the surface of the eye. Further treatments may be indicated if any of these conditions are present.
It is important to realize that without appropriate treatment KCS can result in blindness. When managed properly, animals with KCS can still lead happy, healthy lives!!!!
Epistaxis
by Vani Poosapati
The medical terminology for nose bleeding is epistaxis. Bleeding from the nose can range from some blood tinged droplets sneezed on to the floor to a steady inexorable bloody drip from both the nostrils. There are quite a few diseases that cause nose bleeding. Many are serious diseases and not all the conditions are localized to the nose. Pets with a bloody nose are likely to swallow the blood, which may lead to black stool or even vomit with blood clots in it. To find the cause of the nose bleed the following tests are usually necessary. The initial tests are routine blood work, urinalysis, platelet (a blood cell involved in the clotting) count and blood clotting times. Some diseases cause nose bleeding, because of abnormal clotting times, some other diseases cause nose bleeding because of decreased platelets. If the basic blood work and clotting times are normal, then blood pressure and chest X rays should be taken. Blood pressure measurement is important because high blood pressure causes nose bleeding. Chest X rays help to rule out fungal diseases and cancers of the lungs. If these tests come back as normal then the animal should be anesthetized to perform X rays of the nose, good oral and nasal passage examination. These tests help in diagnosing a tooth root abscesses or growths in the nasal passages. If none of the above tests are helpful in diagnosis then the pet should be seen by referral hospitals for special tests like CT scan of the head and rhinoscopy. Rhinoscopy is visualization of the inside of the nasal passages with the help of a small camera. Rhinoscopy plays an important role in the diagnosis. This is because it is possible to collect samples of any abnormal discharge or growths during the procedure. The evaluation of these samples usually leads to diagnosis.
Flatulence in Dogs and Cats
by Lee Wright
Flatulence occurs when gas from the intestines passes through the anus. Flatulence is also known as “farting” or “passing gas.” Some amount of flatulence is normal in our pets, and it occurs more commonly in dogs than cats. However, some pets may be excessively flatulent. This is most often related to diet. Some pets may not tolerate certain ingredients in their food. For instance, many dogs and cats are intolerant of the lactose present in dairy products. Cutting out any table scraps your pet may receive is advisable. Also, changing to a higher quality or premium diet with more easily digestible nutrients can often help resolve excessive flatulence.
Other causes of excessive flatulence include overeating and eating too quickly (which results in the gulping of air along with food). In some cases, regular exercise can help decrease flatulence by promoting regular defecation.
Although flatulence is usually normal, in some rare cases it may be related to disease. You should consult your veterinarian immediately if your pet has other clinical signs of illness (such as depression, vomiting, or diarrhea). You should also be sure to call a veterinarian if your pet seems uncomfortable due to flatulence or if dietary changes and exercise do not result in improvement.
Flea Control
“I don’t see any fleas on my pet. Why should I be concerned about flea control?”
By the time you notice your pet scratching and consider he may have fleas, the fleas probably are not there! Your pet can easily start to scratch and relocate or eat the fleas. When a flea bites, it deposits its saliva into your pet. Some pets have an allergic reaction to this called flea allergy dermatitis. The itching and irritation can last up to two weeks after the last flea bite—another reason you may not see fleas. As your pet is frantically trying to destroy these fleas, he will in the process end up swallowing some, which increases his risk of acquiring the tapeworm Dipylidium caninum.. Your family can also end up swallowing the fleas—children are more susceptible than adults. Once the fleas are brought indoors by your pet, they then infest your home where they live in the carpet or between the cracks of a wood floor. They wait for a host to jump on to and begin feeding immediately. They may even bite you! The best way to treat these situations is to prevent them. There are several flea products available to prevent flea infestation of your pets. There are also several products to treat your home and your yard.
As mentioned above some pets may have an allergic reaction to flea saliva called flea allergy dermatitis. The cornerstone treatment of flea allergy dermatitis is the removal and prevention of fleas. Some of the available products are:
Frontline (available as a spray or top spot)
- Very effective in control/elimination of flea infestations
- o 100 % reduction in fleas within 24 hours
- Targets multiple stages of flea lifecycle o Kills adults, eggs and larva
- May be used as sole method of treatment of fleas without the aid of premise treatments
- Recommended to apply 48 –72 hours before or after bathing
- Very safe – the mechanism of toxicity only targets fleas and not dogs or cats
- Also effective against ticks
Advantage (topical) Revolution (topical)
- Provides a rapid decrease in adult flea population
- 100 % reduction in adult fleas within 24 hours
- Effective elimination of adult fleas
- Partially removed by swimming and bathing – reapplication may be necessary if animals shampooed regularly
Revolution (topical)
- Prevents and controls flea infestation o Kills adult fleas o
- Decreased flea numbers on dogs by 83% by 24 hours and > 99% at 36 hours; Cats: >98 % at 24 hours
- Not effected by bathing
- Additional effects:
- Prevents heartworm disease, treats and controls ear mites.
- Treats and controls sarcoptic mange in dogs.
- Controls ticks in dogs
- Treats roundworm and hookworm infections in cats.
There are numerous flea products available over the counter (flea collars, topical applications, and flea baths). There are numerous disadvantages to over the counter topical flea applications that include increased flea resistance and potential toxic effects especially to cats. Flea shampoos are not very effective because of the lack of residual activity on animals.
Environmental control:
- Vacuum all carpets
- Vacuum bag should be immediately discarded in outdoor trash
- In severe infestations the carpets may require professional steam cleaning to eliminate eggs
- Wash all pet and human bedding
- Dry laundry on highest heat setting
- Premise spray insecticides may be used to treat outdoors
- Insect growth regulation (IGR) house sprays available (ex. Mycodex home spray)
In severe cases of flea allergy dermatitis, additional medications may be necessary. Steroids can be prescribed to provide immediate relief to itch and discomfort associated with allergic reaction. Additionally antibiotics may be necessary to treat secondary bacterial skin infections.
It may take months to completely rid your pet and your home of a flea infestation. Please contact your veterinarian with any questions or concerns.
Glaucoma- an Emergency for Your Pet’s Eyes
Glaucoma is a condition of increased pressure within your animal’s eyes. It should be considered an emergency because if left untreated, it can lead to permanent blindness in as little as 12 hours!
There are several signs of glaucoma that you may notice at home. Early on, your pet may blink more often, shy away more obviously from hands, have a red looking eye, have a protruding third eyelid, or even be showing signs of blindness already. As the condition is present for a longer time, the eye may appear more reddened (with more serious pain), the cornea may be more cloudy or even opaque, the pupil will be dilated, and signs of blindness are more likely to be present. If left untreated for longer than a few days, the pain may decrease somewhat, but it will probably never go away. At this stage blindness and increased size of the eye are almost always permanent.
If you suspect any signs of glaucoma are present in your pet, it is important to see a veterinarian immediately. The sooner you seek treatment, the more likely it is that your pet may retain its vision. A veterinarian can measure the pressure within your animal’s eye and determine the seriousness of the condition. It is also important to start immediate medical therapy to reduce inflammation and pressure within the eye. If your pet’s eyes respond to medical therapy, and treatment is started early enough, the prognosis for vision can be good.
There are multiple causes of glaucoma. Several breeds of dog are predisposed to glaucoma including Beagles, Cocker Spaniels, and Samoyeds. Glaucoma can also be secondary to several other conditions such as an eye tumor, inflammation in the eye, and trauma. Ask your veterinarian if you have questions about this vision threatening condition
Have a Safe Trip
A responsible pet owner knows the importance of bringing their pet to the veterinarian for wellness exams or when they are sick. Transporting an animal from its home environment to the veterinarian can be somewhat of a daunting task however. The following are a few suggestions to make the process run smoothly.
- DOGS – Please make sure that the dog is wearing a harness or collar and is on a leash. ID tags should be attached to the harness or collar, in the event that they escape. A crate or dog seat belt helps to keep the dog secure in the car.
- CATS – Please make sure cats are in a carrier. They may seem reluctant to go in it at home but often appreciate the security it offers once at the hospital.
- BIRDS – Small birds can be transported in their cages, but please make sure it is covered if the weather is inclement. Larger birds can be transported in carriers used for cats.
- EXOTICS – Other animals such as ferrets, rabbits and iguanas also benefit from the safety provided by a carrier.
- POCKET PETS – Small mammals such as hamsters and gerbils can be transported in their cages or in one of the small plastic transport containers sold in stores.
The goal is to keep the pet safe and comfortable during the trip. If you have any questions about what the best way to transfer your pet is, please do not hesitate to call your veterinarian. Have a safe trip!
Why Test for Heartworm Disease Differently in Dogs and Cats
by Laura Smith
Heartworm disease acts very differently in dogs and cats. Dogs are the definitive host for heartworm disease. This means dogs get an immature form of the worms from a mosquito, and the worms then mature to adults and reproduce in the dog. The cat is an aberrant host of heartworm disease. This means the worms do not normally mature or reproduce in cats and there are usually less worms present in cat heartworm disease then dog heartworm disease.
There are three blood tests that are routinely used to detect heartworm disease in small animals. The first is an occult heartworm test. This test is used in dogs that receive heartworm preventative during the mosquito season or ideally year round (Heartgard, Interceptor, Sentinel, Revolution, and Pro-Heart 6) and in dogs that are not on heartworm preventative. The test detects if there are adult heartworms present in the dog’s body by detecting proteins, or antigens, released by mature female heartworms. Since dogs with adult heartworms usually have lots of mature worms, there is usually a lot of antigen present to be detected. If a dog has a positive occult test, it has adult heartworms in its heart and/or pulmonary arteries. If a dog has a negative occult test, it does not have adult heartworms. Cats, on the other hand, rarely have greater than 6 worms, and the worms are much more likely to be immature or only male in cats. If a cat has a positive occult heartworm test, it has heartworm disease, but if it has a negative occult test, it may or may not have heartworm disease.
The second heartworm test is a microfilaria or modified Knott’s test. Microfilaria are larval or immature forms of heartworms. Dogs are much more likely to have microfilaria than cats, since heartworms readily reproduce in dogs. Microfilarial tests detect larval heartworms that are either given to a dog from an infected mosquito or produced from adult heartworms living in the dog. Heartworm preventatives kill or prevent maturing of microfilaria, so this test is not performed on dogs receiving preventative. However, this test is performed on dog’s that have not been on heartworm preventative for 6 months or longer. The test is performed because a dog could have microfilaria without having adult worms if the dog was bitten by a mosquito carrying heartworm disease and the microfilaria have not had enough time to mature to adult heartworms.
The third heartworm test is an antibody test. This test determines whether or not an animal has made antibodies against heartworm antigens. The test only tells veterinarians if the animal has been exposed to heartworms. It does not tell veterinarians whether or not an animal has a heartworm infection in its body. This test is not used in dogs because the occult and microfilarial tests are inexpensive and reliable ways to determine if a heartworm infection is present. However, this is the preferred test in cats, because the other methods are not sensitive enough to determine if heartworm disease is present in cats. A negative antibody test means the cat has never been exposed to heartworms and does not have heartworm disease. A positive antibody test means the cat has been exposed to heartworms, but may or may not have the disease right now and further tests are needed to determine if the cat has heartworm disease.
It is very important that all cats be kept on heartworm preventative. Cats that are infected with heartworms may only have a few worms. However, when these worms die, they are much more likely to be lodged somewhere in the body, which can cause very severe signs in the cat. It is common that the first sign seen in a cat with a heartworm infection is death. Even indoor only cats may be at risk, if a mosquito slips in an open door or a torn screen.
Hyperparathyroidism in Dogs and Cats
by Jennifer Scott
Normal calcium regulation in your pet is taken care of by a balance of two hormones that work against each other to keep calcium from being too high or too low. The hormone called calcitonin keeps calcium from getting too high and parathyroid hormone produced by the parathyroid gland keeps calcium levels from getting too low. Hyperparathyroidism is the term used when the parathyroid gland produces more of the parathyroid hormone than it is supposed to. This can happen because of a problem with the parathyroid gland itself or from a secondary problem somewhere else in the body. When too much parathyroid hormone is released, too much calcium is released into the blood. For the body to get this calcium into the blood it has to take stored calcium from bones. This leads to bone resorption, which can cause weakening and fracture of bones even when no trauma was present. When there are secondary problems causing the parathyroid gland to work overtime an animal may have signs of that secondary disease. For example, some animals with kidney disease will develop hyperparathyroidism as a complication and in those pets signs of kidney failure such as vomiting, dehydration, increased drinking and urination, and depression can appear first. Hyperparathyroidism can be diagnosed by a simple blood test for calcium and parathyroid hormone levels. Treatment depends on any underlying conditions your pet may have and whether the problem is with the parathyroid gland itself or is secondary to other problems in the body (i.e. kidney disease). If the problem is with the parathyroid gland then surgery to remove the gland may be needed. If the problem lies elsewhere, further testing may need to be done to find the best treatment for your pet.
Hyperthermia (Heat Stroke)
Hyperthermia is defined as an excessively high body temperature of 105-110 ºF. The problem occurs most commonly during the summer when the temperature is high along with a high humidity. It is this Heat Index that is the most important factor for heat stroke.
Dogs and cats cannot sweat like people and so they pant to release the heat. The only place a pet can sweat is from their foot pads. Your pet should be provided plenty of shade. It is important to remember that this shade will change throughout the day so a shady spot should be made available at all times. You pet should be provided plenty of fresh water at all times. You should not over exercise your pet on days when the heat index is high. A small child swimming/wading pool filled with fresh water can be used as a cool down source.
Your pet should never be left in a car unattended. On a cool day of 75ºF, the temp. inside a car can soar to 120 ºF in only 10 minutes. Even leaving your windows open does not allow the air to circulate properly to reduce the risk of heat stroke.
Signs of Heat Stoke:
- Excessive panting
- Excessive Salivation (drooling)
- Racing pulse
- Legs, ears, nose hot to the touch
- +/- vomiting
What to do if you think you pet is suffering from Heat Stroke?
- Have a pet thermometer to take your pet's temperature
- Bring inside to Air Conditioning
- Place in a cool water bath - offer sips of cool water
- Contact your regular veterinarian immediately!
Pilling Your Pet
While many dogs and cats, as well as other household pets, are always ready and willing to take their oral medications, you may end up discovering that your pet may be quite challenging. Here are several methods that may help alleviate the headache that could arise from an oral prescription for your pet:
- “Open and insert” is the most basic and simplest method to use if your pet will allow. Simply pull the mouth open and drop the medication on the back of the tongue. Some animals may need their muzzle held shut for a few seconds to ensure swallowing of the pill rather than spitting it out.
- Disguising the pill in a treat may be a valid option if you have an animal that resists working in or around the mouth. Placing pills in hotdogs, meatballs, and peanut butter are tricks commonly used. Cheese cubes also seem to work very well as the animal is less likely to discover the pill and work it out. (Be sure to observe the animal eating the entire treat and make sure they don’t walk away while still chewing. Some are very good at spitting the pill out elsewhere!)
- Oral suspensions are another option for the animal that refuses to swallow tablets or capsules (if the prescribed drug is available in oral form). Using a syringe or medicine dropper, place the tip underneath the lip on the side of the mouth. It usually works better to quickly squirt in most of the medication and let the animal lick and swallow rather then trying to force in a few drops at a time. Most capsules and tablets may also be dissolved in water and given via syringe, alleviating the need to place one’s hands in an unwilling animal’s mouth.
- If capsules are being given and the pilling method is not agreeing with the animal, the capsule may be opened and the powder within is sprinkled over a treat or mixed in with a small amount of dog food. Make sure to allow the animal to only have access to this small amount of food until all the medication is consumed before feeding the animal the rest of the meal.
- Over time, your sweet innocent pet may become a master of trickery to combat you in the ongoing battle of pilling. Some dogs even get to the point of allowing you in their mouth, placement of medications on the back of the tongue, but still refuse to swallow. A good trick to outwit your pet here is that once the pill is in the mouth, hold the mouth shut and squirt a small amount of water into the mouth from the side under the lip (same as above using a syringe or dropper). This should stimulate your pet to swallow and the pill goes down usually unnoticed.
Pets and their owners are both evolving new ways to pill and overcome being pilled. It is most important to try different methods with your pet and to administer medications to your animal in the least stressful, simplest, and safest way for both you and your pet.
Always ask your veterinarian before cutting, crushing, or dissolving your pet’s medication. Some medications are less effective if the whole tablet or capsule is not given.
Senior Pet Wellness: The Doggone Best Prevention
by Dr. Steve Thompson & Dr. Lorraine Corriveau
Senior Pet Wellness is a critical lifestage that has not always been emphasized appropriately as some practices seek to develop prevention programs for the aging pet population. Just as the 65 year old person recognizes they are now senior citizens and eligible for their golden years' benefits, they don’t usually consider themselves geriatric. Many common screening tests begin late adult, early senior life in people. Some common ones include cholesterol screening, prostate exams, colonic exams and mammography screening. Previous family histories of some of these health concerns may prompt an earlier testing cycle or more frequent screenings when warranted. While most people can accept some initial wellness screening at these senior ages, they may not feel up to a battery of geriatric lab tests or feel it is appropriate. This has certainly been the case for some practitioners trying to implement Geriatric programs into their practices. Establishing age 6 or 7 as a magical, perhaps arbitrary, cut off for beginning these tests, pet owners have sometimes balked at the idea of needing to spend $150 on testing for their 7 year old dog when nothing was done the previous year. To them, their dog or cat hasn’t changed much and they are probably right!
We experienced a similar situation to that described above related to pre-anesthetic screening at Purdue. While a CBC and urinalysis was our comfort level for pre-dental workups prior to age 6, we added a full chemistry and chest rads at age 7 and owners began to question why the dental costs increased over $150 (50%) in a single year. Once again, to them the dog essentially looked and acted the same, had dental tartar with mild gingivitis like last year and yet necessitated substantially higher workup costs. While we have begun doing a good job of educating our owners to the idea of wellness care, they ask really good questions. Incidentally, so do our veterinary nurses and students! In consultation with our surgeons and anesthesiologists, we have modified our pre-anesthesia workups to mimic our phased in approach to pet aging and wellness screening.
Wellness services for senior or mature pets should include the same general categories as identified for adult pets. Physical examination findings, nutrition assessment, oral health, infectious disease screening and prevention, parasitic disease screening and prevention, behavior and lifestyle concerns related to the pet, behavior and lifestyle concerns related to the family, zoonotic and societal concerns related to public health, reproductive health concerns and genetic health concerns. Degenerative and aging health concerns are now part of the wellness discussion during these later year visits with a more aged patient. For continuity sake, we use the same Wellness form as we began using after the pet turned 4 months old. Introducing a phased in approach to senior pet wellness screening has been much more successful for us as we work with pet owners, compared to suddenly launching a geriatric program. Clients seem to feel there are more standard recommendations when we put them in black and white and we feel they are now more aware of what services are available to their pets. What follows are some comments related to wellness visits for the senior pet years.
The Exam. The physical exam remains the most important foundation for overall wellness care and valuing veterinary expertise and services. I continue to highlight normal parameters during the physical exam, noting that the pet appears to be “aging gracefully.” When appropriate, I think it is often helpful to relate an appropriate age conversion for their pet. While we view 7 years as still a young child, we realize that this is already passing the half way point of the life expectancy for most large or especially giant breeds. Calculations exist that allow you to determine an actual age based on body weight and human life expectancy. Often it is just as feasible to use 75 years as a human parameter (for women a little longer than men…) but we should account for the first two years being about 25 years of life. That leaves 50 human years to be divided by the life expectancy of that sized breed. Commonly, in 2009, we use 14-16 for cats and small dogs, 12-14 for large breed dogs and 9-10 for giant breed dogs. It is important to identify minor abnormalities that are abnormal yet may not require intervention. Common examples in senior pets include lenticular sclerosis (and differentiating it from cataracts), iris atrophy which may result in poor pupil light responses, missing teeth, and sagging skin folds that may develop with associated fat deposits or just result from reduced elasticity. Not mentioning these items during a visit may raise questions related to completeness when they are identified by a relative or neighbor in the future or discussed later during a sick pet visit … by another veterinarian. It is especially important to integrate a whole body drawing into the physical exam documents during the senior pet visits. This allows small skin changes and the presence of small growths, lumps and bumps to be easily mapped and described. I encourage owners who are regularly bathing or grooming their pets to begin more closely monitoring the skin for these changes.
Body condition scoring. “Feed to feel” is still the best recommendation that I give to clients. Lifestyle issues here may not necessitate changing all 7 year old pets onto diets with moderate protein, less fat and more fiber. Working and hunting dogs, in their prime, will still need higher carbohydrate foods, especially prior to events. Lower fat diets may occasionally contribute to a worsening of seborrhea sicca (dry skin), especially during lower humidity months in northern climates. It is still appropriate to discuss hair coat quality, stool consistency or volume, flatulence or housebreaking concerns if dietary modifications to premium diets are advisable. We still recommend 40-45 minutes of daily exercise with their pets so that it promotes trimmer pets and owners. Observations of exercise intolerance, reduced playfulness, lameness, coughing or respiratory distress are all key discussion items for owner awareness.
Dental Care. Most pets will need annual or biannual dental prophies between the senior ages of 7 and 11 years. The economic issues of annual dentistry, more advanced lifestage screening and pre-anesthetic screening requires figuring out ways to make this economically feasible for most pet owners. We will continue to phase in the metabolic screening that is age and breed appropriate. Other services can continue to be accomplished while under anesthesia. Common medical services that can be considered during this anesthetic event include removal of skin or eyelid tumors, especially those in readily visible or conspicuous places. Wellness and pre-anesthetic screening of these patients usually requires running a couple small lab tests. Semiannual wellness exams can be prioritized. All items are covered on the wellness exam sheet with most of the owner costs going into infectious disease and parasite detection and control at one visit. The follow-up exam 6 months later allows time and budgets to better assess oral health, nutrition and behavior issues. This visit is primarily run by our nutrition, behavior and dentistry nurses, with input from the doctors if medical concerns exist or anesthesia is necessary. Our hope is that by spreading out the costs of the dental to 6 months later, pet owners will be more readily able to proceed with the dental cleaning at these times. We hope to more accurately evaluate weight loss (or gain), and intervene earlier on behavior or lifestyle concerns.
Pre-anesthestic screening. On top of CBC and Urinalysis needs in the 6-7 year old pet, we add a mini chemistry panel. Currently this includes liver (ALT, AlkPhos, GGT) and kidney (creatinine) parameters in addition to Glucose. Between ages 8-10, we do a full chemistry panel. Giant breed dogs would have this earlier. Baseline T4 levels are being done in cats over age 8 and in dogs over age 10. TSH assays allow us to readily differentiate sick euthyroid cases from hypothyroid cases in older dogs. Certainly pets with medical concerns would have appropriate workups done when necessary. The guidelines I am discussing relate to the senior pet with a normal physical exam preparing for elective anesthesia for dentistry and/or growth removal. Depending on the presence of heart murmurs, chest rads are not routinely added to our preanesthetic workup until the patients reach age 10. We are not currently utilizing blood pressure screening in our senior pet group due to the dramatic variation noted in values and low incidence of primary hypertension in dogs and cats. Electrocardiograms are monitored on all patients under anesthesia, young and old, but screening ECG’s won’t usually modify our anesthetic protocols unless arrhythmias were ausculted during the initial physical exam. Recently, it appears that the presence of VPC’s on screening Dilated Cardiomyopathy occurring within 2 years of the initial identification of rare ventricular beats. Applicability to other breeds that get DCM may apply and we are looking at utilizing this screening test in appropriate breeds.
Infectious disease screening. It is important to assess heartworm status on an annual basis in regions where heartworm prevalence is high (over 5%). Even in low prevalence areas where biannual testing is done, it is critical to screen all one year old dogs as well as all pets acquired through rescue and shelter environments. The test does not pick up recent infections but assesses any missed doses from 6 months or more prior to the test. Our most common positive dogs are dogs who were negative on an initial shelter or rescue test, yet currently infected with early stage larva, that the test picks up the next year once these larva mature. Heartworm preventives are not completely effective once the larvae are past 45 days. Early detection of infections allows treatment before significant, irreversible cardiac or respiratory disease develops.
Genetic screening. Risk factors affecting senior pet wellness also include breed related disorders, particularly in dogs. By this age, we are encouraging even our responsible breeders to decide on when they will have their last litters. We then have their pet neutered to prevent pyometra and testicular tumors. I tend to have little tolerance for pet producers still “on the fence” about breeding when we get into this age group. Genetic screening continues for glaucoma in at risk breeds as before, on an annual basis. Orthopedic screening of hips that may not have been done at an earlier visit will often by coincided with a dental anesthesia, esp. if there are any concerns about rear weakness or slowing down in the hindend. Unique screenings may apply for selected breeds as DNA testing becomes more readily available and for specific breed concerns. Topics we are actively looking into relate to breeds prone to cystic calculi (taking an abdominal radiograph) and breeds prone to bladder cancers (single organ ultrasound) may be warranted since a urinalysis does not always detect disease in these patients. Other areas include Schirmer tear testing of at risk breeds and thyroid autoantibody testing of at risk breeds. Many more options may be present as we look into specific breed related problems that manifest themselves later in life. Relating back to eye care however, the question has been raised as to what really qualifies as a wellness eye exam and is direct ophthalmoscopy providing an appropriate wellness exam of the fundus. With the fundus serving as a window to the body, it seems prudent to examine how frequently we must dilate a pet’s eyes and do an appropriate indirect exam. At the least, it would seem that the senior pet years are a good time to get into this habit since lenticular sclerosis is already obscuring somewhat limited access through a nondilated pupil.
Lifestyle and Behavior. Issues related to owner, family and pet lifestyle should still be evaluated to determine appropriate vaccination strategies. Owners are hopefully now aware of behavior consultation availability in veterinary practices or affiliated with the practice. Many of the initial playful, distracting, annoying and aggressive behaviors have been overcome by this age although aggression may be attributed to irritability related to dermatologic or orthopedic health concerns. Housebreaking concerns should never be chalked up to aging function without appropriate work up for conditions related to either increased appetite and increased stool production or increases in drinking or urination. As the pet enters its senior years, it still may present with new anxiety and phobic disorders. Initial age of onset is often biphasic with a juvenile onset and senior/geriatric onset documented. Concurrent behavior conditions should always be evaluated with appropriate neurologic, cardiac, endocrine and metabolic assessments. Monthly or quarterly metabolic, cardiac or tonometric monitoring is usually necessary if pets are maintained on anxiolytics.
Taking Your Pet with You on the Road
by Dawn Haas
Before the Trip
Traveling with your pet can be a fun experience as long as some planning is done before embarking on your journey. It is important to assess your pet’s health before taking them on a long car ride. If you are concerned about your pet’s ability to travel with you it may be better to hire a pet sitter or find a kennel rather than risking their health by taking them with you. To better assess your pet’s ability to travel, an appointment with your veterinarian is suggested. At this time you can ask about any flea, heartworm, tick or other infectious disease risks in the areas where you will be traveling. It is also important to be sure that all vaccinations are up to date as well as heartworm, flea and tick prevention. It is important that your pet always wear a collar with up to date rabies tags, name, address and phone number. It is also advisable to make temporary tags with the address and phone number at your destination. Having your pet microchipped can also be beneficial in case your pet becomes separated from you during the trip. Before taking a longer trip, try a series of shorter trips to be sure your pet is use to traveling in the car. The morning of a long trip feed a light meal. A meal of 1/3 the usual amount can be fed before leaving with the remainder being fed when reaching your final destination.
On the Road
Once on the road, you should never let your pet ride unrestrained in the car. Either a pet seat belt or a secured carrier should be used. These can help prevent severe injury to your pet in the case of an accident. A carrier should be large enough for your pet to stand up, turn around and lie down comfortably. It should also be leak-proof, well ventilated, free of protruding objects and have a door that latches securely. Never allow your pet to wear a choke or pinch collar while traveling as these can become caught on objects and can result in serious injury. Breaks should be taken at least every three hours to let your pet exercise and relieve itself. Never leave your pet alone in the car, especially in extremely hot or cold weather.
With some simple planning, traveling with your pet can be an enjoyable experience for everyone involved. Contact your veterinarian with any questions.
Trimming Your Pet’s Nails
Preparation is important, because many dogs and cats do not like their paws to be touched. It is best to start touching their paws when they are as young as possible, so that they get used to it. When beginning this process, start slowly by getting them used you touching a paw, then gradually holding on to it for longer periods of time. Treats may be used to reward them for not pulling the paw away. With a cat, also practice extending the claws, before you are trying to cut them. When they will let you hold their paw, it is time to start introducing the clippers. Reward the animal for being calm with the clippers on the floor in sight, gradually move them closer to the animal. This should be done, because some animals will run and hide even at the sight of the clippers, especially if they have had a bad experience. Again, go slowly and reward them for holding still. Don’t expect to trim all the nails at once the first time.
The nail has an outer part which is safe to cut, and an inner part, called the quick, which contains nerves and blood vessels. When ever clipping your pet’s nails you should have styptic powder available to stop any bleeding that occurs. Try not to clip your pet’s nails short enough that they bleed, but accidents happen, and you should be prepared to stop the bleeding. Hold the paw in a comfortable position, with the dog lying down or the leg supported under its body. If the dog is off balance, it will resist more. In white nails, the quick can easily be seen and avoided, but black nails are harder.
There are several guidelines which can be used:
- Trim a little at a time.
- The nail can be cut where it curves and comes level with the pad. However, caution must be used when cutting nails which have grown for a long time, because the quick grows further out in the nail.
To trim your cat’s nail you will need to extend the nail by pushing down just behind the base. Human nail clippers are often used to trim cats’ toenails (as seen below). Be sure to trim only the sharp point, this will help ensure that you avoid the pink quick and do not cause bleeding and pain. You should trim your cat’s nails every 1‐3 weeks because cats shed their nails and replace them with sharp new ones rapidly. If you have any questions or concerns contact your veterinarian.

This picture shows a dog toenail. The yellow line indicates where the nail should be cut.
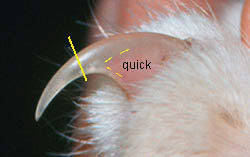
This picture shows a cat nail. The yellow line indicates where the nail should be cut.

This picture shows a cat nail being clipped.
Understanding your pet’s blood work
Blood tests help us determine causes of illness accurately, safely, and quickly and let us monitor the progress of medical treatments. A checkmark in any box indicates a significant abnormal finding on your pet’s blood work. If you have questions, ask any staff member. We want you to understand our recommendations and be a partner in your pet’s care.
Complete blood count (CBC)
The most common blood test, a CBC gives information on hydration status, anemia, infection, the blood’s clotting ability, and the immune system’s ability to respond. This test is essential for pets with fevers, vomiting, diarrhea, weakness, pale gums, or loss of appetite. If your pet needs surgery, a CBC can detect unseen abnormalities.
- HCT (hematocrit) measures the percentage of red blood cells to detect anemia and dehydration.
- Hb and MCHC (hemoglobin and mean corpuscular hemoglobin concentration) measure hemoglobin, the oxygen-carrying pigment of red blood cells (corpuscles).
- WBC (white blood cell count) measures the body’s immune cells. Increases or decreases indicate certain diseases or infections.
- GRANS and L/M (granulocytes and lymphocytes/ monocytes) are specific types of white blood cells.
- EOS (eosinophils) are a specific type of white blood cells that if elevated, may indicate allergic or parasitic conditions.
- PLT (platelet count) measures cells that help stop bleeding by forming blood clots.
- RETICS (reticulocytes) are immature red blood cells. High or low levels help classify anemias.
Blood serum profile
These common tests evaluate organ function, electrolyte status, hormone levels, and more. They are important in evaluating the health of older pets, pets with vomiting and diarrhea or toxin exposure, pets receiving long-term medications, and preanesthetic patients.
- ALB (albumin) is a serum protein that helps evaluate hydration, hemorrhage, and intestinal, liver, and kidney health.
- ALKP (alkaline phosphatase) elevations may indicate liver damage, Cushing’s disease, and active bone growth in young pets.
- ALT (alanine aminotransferase) is a sensitive indicator of active liver damage but doesn’t indicate the cause.
- AMYL (amylase) elevations show pancreatitis or kidney disease.
- AST (aspartate aminotransferase) increases may indicate liver, heart, or skeletal muscle damage.
- BUN (blood urea nitrogen) reflects kidney function. An increased blood level is called azotemia and can be caused by kidney, liver, and heart disease, urethral obstruction, shock, and dehydration.
- Ca (calcium) deviations can indicate a variety of diseases. Tumors, hyperparathyroidism, kidney disease, and low albumin are just a few of the conditions that alter serum calcium.
- CHOL (cholesterol) is used to supplement diagnosis of hypothyroidism, liver disease, Cushing’s disease, and diabetes mellitus.
- Cl (chloride) is an electrolyte often lost with vomiting and Addison’s disease. Elevations often indicate dehydration.
- Cortisol is a hormone that is measured in tests for Cushing’s disease (the low-dose dexamethasone suppression test) and Addison’s disease (ACTH stimulation test).
- CREA (creatinine) reveals kidney function. This test helps distinguish between kidney and nonkidney causes of elevated BUN.
- GGT (gamma glutamyl transferase) is an enzyme that when elevated, indicates liver disease or corticosteroid excess.
- GLOB (globulin) is a blood protein that often increases with chronic inflammation and certain disease states.
- GLU (glucose) is blood sugar. Elevated levels may indicate diabetes mellitus. Low levels can cause collapse, seizures, or coma.
- K (potassium) is an electrolyte lost with vomiting, diarrhea, or excessive urination. Increased levels may indicate kidney failure, Addison’s disease, dehydration, and urethral obstruction. High levels can lead to cardiac arrest.
- LIP (lipase) is an enzyme that may indicate pancreatitis when elevated.
- Na (sodium) is an electrolyte lost with vomiting, diarrhea, and kidney or Addison’s diseases. This test helps indicate hydration status.
- PHOS (phosphorus) elevations are often associated with kidney disease, hyperthyroidism, and bleeding disorders.
- TBIL (total bilirubin) elevations may indicate liver or hemolytic disease. This test helps identify bile duct problems and certain types of anemia.
- TP (total protein) indicates hydration status and provides information about the liver, kidneys, and infectious diseases.
- T4 (thyroxine) is a thyroid hormone. Decreased levels often signal hypothyroidism in dogs, while high levels indicate hyperthyroidism in cats.
Valley Fever (coccidiodomycosis) in Dogs
Valley Fever, or coccidioidomycosis, is caused by the soil dwelling fungus Coccidiodes immitis. The disease is seen primarily in semi-arid areas such as Arizona, California, New Mexico, Texas and parts of central and South America. Animals (including humans) traveling through these areas are at risk of being exposed. Valley Fever is considered to be noncontagious from animal to animal except for the potential of contracting infection through draining skin lesions. The organism prefers acidic environments and is commonly found around the entrances to gopher and ground squirrel dens because of their urine. The incidence of disease increases in late summer and fall, or when human and dust-disturbing events (windstorms, construction) send dust into the atmosphere. C. immitis is inhaled from the environment and concentrates in the lungs, but has the ability to spread to other parts of the body. Young, large-breed dogs are most commonly affected, but cats and small dogs are susceptible too.
Many dogs are not obviously sick, or may have vague symptoms that are not recognized by owners. These animals often overcome disease without receiving treatment. Many dogs also however, develop symptoms approximately three weeks after infection. The primary infection is localized to the lungs and symptoms include cough, fever, depression, lack of appetite and weight loss. In some dogs, disseminated disease may occur which most commonly affects the skin, bones and joints. In severe cases, the disease can spread to the eyes or to the brain and cause seizures.
Clinical symptoms, diagnostic tests and travel history are equally important in diagnosing Valley Fever. Diagnostic testing includes blood tests and x-rays of the chest and bones that are swollen or painful. The blood tests include an antibody test often referred to as a “titer” that looks for increases in specific antibodies for Valley Fever. Titers are often negative in early disease, and may need to be repeated in one month.
Treatment of Valley Fever requires the use of antifungals which most commonly include ketoconazole, itraconazole and fluconazole. The course of treatment is usually extensive and ranges from six months of medication to lifelong management. Animals with more severe disease (bone or brain involvement) usually require treatment of longer duration. Most dogs with clinical signs of Valley Fever, recover with appropriate and diligent treatment.
What is this Lump?
There may come a time in your pet’s life when you may notice a lump or bump. When you see these lumps or bumps, there are many things that your veterinarian may be able to do to determine what this lump or bump may be. Some important questions that you may be asked when you take your animal to the vet include:
- When did you first notice this lump or bump?
- Could this lump or bump be the result of a traumatic incident?
- What was the color of this lump or bump when you first noticed it?
- What was the consistency of the lump or bump when you first noticed it (was it hard, soft, freely movable, attached to the underlying tissues)?
- What was the temperature of the lump or bump when you first noticed it (was it cold or warm)?
- Has the size of the lump or bump changed since you first noticed it?
- Has there been any change to the outside surface of the lump or bump, such as a change in color, any ulceration of the skin, has there been any discharge from the lump or bump, etc..?
- Does the lump or bump seem to cause your pet pain? Has the number of lumps or bumps changed since you first noticed them? Has your pet been vaccinated in the area of the lump or bump?
It may be a good idea to map and measure any lumps or bumps when they are first found in order for progression of the lump or bump to be evaluated at a later point in time.
There are many things that your veterinarian can do to try to determine the cause of your pet’s lump or bump. First, they will try to answer 2 key questions:
- What is it?
- How far has it spread?
Some tests that your veterinarian may want to perform in order to answer these questions include:
- Physical exam Routine bloodwork such as a complete blood count, serum biochemistry, and Urinalysis
- Palpation of the lump or bump and regional lymph nodes
- Map and measure the lump or bump
- Fine needle aspirate of the lump or bump and regional lymph nodes
- Tru-cut biopsy of the lump or bump
- Radiographs of the chest and abdomen
- Ultrasound of the abdomen
- Bone marrow evaluation through aspiration or core biopsy
At some point throughout this myriad of tests, your veterinarian will most likely come to a diagnosis. At that time, a decision regarding the care and treatment of this lump or bump will need to be made. Some possible treatment options for many types of lumps or bumps include surgical excision, radiation therapy, chemotherapy, or a combination of any of the three.
Remember that observation is one of the best tools that we own in the black bag we call veterinary medicine.